VA Cited for Neglecting Follow-Up Treatment for Depressed Vets

The embattled Veterans Affairs Department is once again under scrutiny for potentially violating agency guidelines when treating patients—this time, failing to ensure that veterans with depression are receiving sufficient follow-up care after being prescribed anti-depressant medication.
That’s the conclusion of an investigation by the Government Accountability Office. The GAO reviewed patients being treated for depression at six separate VA medical centers and found that after the veterans received anti-depressants, their doctors did not conduct follow-up appointments within four to six weeks, as the VA requires
Related: VA Wastes Millions, But Still Wants More as Vets Wait for Care
In its review, the GAO said that among all patients whose records were reviewed—almost none of them received check ups with doctors in the required time after they were given anti-depressant medication.
"Given the debilitating effect that depression can have on veterans' quality of life, VA's monitoring of veterans with [depression] is critical to ensuring they receive care that is associated with positive health care outcomes," GAO director of health care Randall Williamson said in congressional testimony this week. He went on to criticize the VA for not following its own guidelines to assure veterans receive sufficient treatment.
“This work illustrates, once again, a continuing pattern of VHA's [Veterans Health Administration] noncompliance with its own policies and established procedures,” Randall Williamson, the GAO's director of health care said in congressional testimony last week.
Separately, the GAP flagged the VA’s Behavioral Health Autopsy Program which is used to collect data on veterans that have committed suicide in order to inform policy decisions, saying it is plagued with inaccuracies.
Auditors said that the system had incorrect dates of death—sometimes off by one day, sometimes off by a whole year. The GAO said this made it nearly impossible to assess what kind of treatment they were provided.
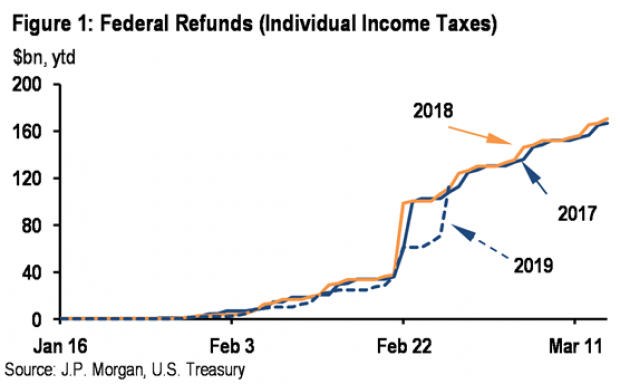
Tax Refunds Rebound
Smaller refunds in the first few weeks of the current tax season were shaping up to be a political problem for Republicans, but new data from the IRS shows that the value of refund checks has snapped back and is now running 1.3 percent higher than last year. The average refund through February 23 last year was $3,103, while the average refund through February 22 of 2019 was $3,143 – a difference of $40. The chart below from J.P. Morgan shows how refunds performed over the last 3 years.
Number of the Day: $22 Trillion

The total national debt surpassed $22 trillion on Monday. Total public debt outstanding reached $22,012,840,891,685.32, to be exact. That figure is up by more than $1.3 trillion over the past 12 months and by more than $2 trillion since President Trump took office.
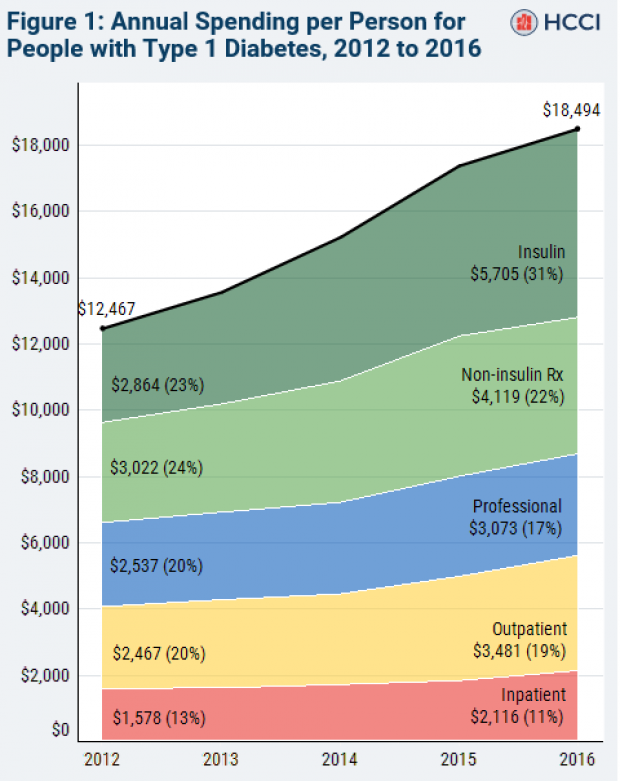
Chart of the Week: The Soaring Cost of Insulin

The cost of insulin used to treat Type 1 diabetes nearly doubled between 2012 and 2016, according to an analysis released this week by the Health Care Cost Institute. Researchers found that the average point-of-sale price increased “from $7.80 a day in 2012 to $15 a day in 2016 for someone using an average amount of insulin (60 units per day).” Annual spending per person on insulin rose from $2,864 to $5,705 over the five-year period. And by 2016, insulin costs accounted for nearly a third of all heath care spending for those with Type 1 diabetes (see the chart below), which rose from $12,467 in 2012 to $18,494.
Chart of the Day: Shutdown Hits Like a Hurricane

The partial government shutdown has hit the economy like a hurricane – and not just metaphorically. Analysts at the Committee for a Responsible Federal Budget said Tuesday that the shutdown has now cost the economy about $26 billion, close to the average cost of $27 billion per hurricane calculated by the Congressional Budget Office for storms striking the U.S. between 2000 and 2015. From an economic point of view, it’s basically “a self-imposed natural disaster,” CRFB said.
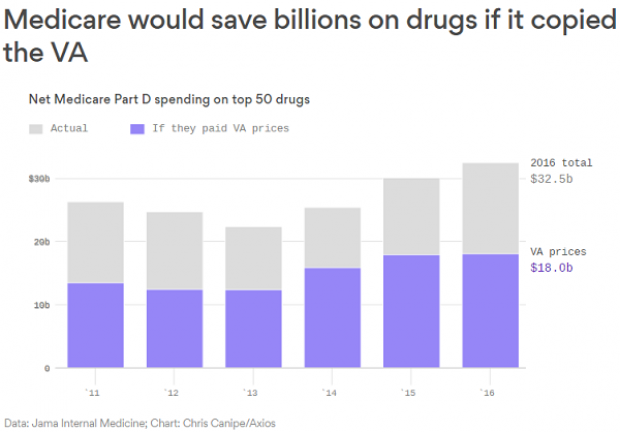
Chart of the Week: Lowering Medicare Drug Prices

The U.S. could save billions of dollars a year if Medicare were empowered to negotiate drug prices directly with pharmaceutical companies, according to a paper published by JAMA Internal Medicine earlier this week. Researchers compared the prices of the top 50 oral drugs in Medicare Part D to the prices for the same drugs at the Department of Veterans Affairs, which negotiates its own prices and uses a national formulary. They found that Medicare’s total spending was much higher than it would have been with VA pricing.
In 2016, for example, Medicare Part D spent $32.5 billion on the top 50 drugs but would have spent $18 billion if VA prices were in effect – or roughly 45 percent less. And the savings would likely be larger still, Axios’s Bob Herman said, since the study did not consider high-cost injectable drugs such as insulin.